

Male Fertility: Low Sperm Count & Sperm Motility
With AIC’s Male Infertility bundle, boost your fertility and unlock your reproductive potential with our scientifically-formulated supplements, designed to enhance sperm quality, motility, and count. Support your journey to fatherhood with our expertly-crafted blend of antioxidants, vitamins, and minerals.
Understanding Male Fertility: Low Sperm Count and Low Sperm Motility
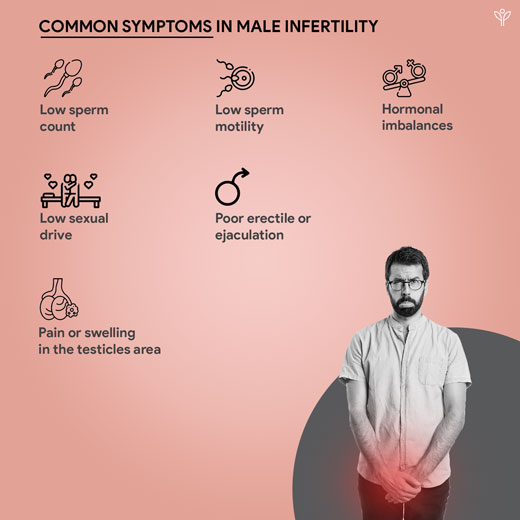
Infertility is defined as the inability to achieve pregnancy after 12 months of regular unprotected sexual intercourse (Cooper et al., 2009). While infertility affects both men and women, male infertility is a significant contributor, accounting for up to 50% of all infertility cases. (Selvam et al., 2019)
Two of the primary factors contributing to male infertility are low sperm count (oligospermia) and low sperm motility (asthenozoospermia). Let’s understand these issues in greater detail.

What we have in Male Fertility: Low Sperm Count & Sperm Motility
Reference
Aitken, R. J., & Baker, M. A. (2006). Oxidative stress, sperm survival and fertility control [Review of Oxidative stress, sperm survival and fertility control]. Molecular and Cellular Endocrinology, 250(1), 66. Elsevier BV. https://doi.org/10.1016/j.mce.2005.12.026
Babakhanzadeh, E., Nazari, M., Ghasemifar, S., & Khodadadian, A. (2020). <p>Some of the Factors Involved in Male Infertility: A Prospective Review</p> [Review of <p>Some of the Factors Involved in Male Infertility: A Prospective Review</p>]. International Journal of General Medicine, 29. Dove Medical Press.
https://doi.org/10.2147/ijgm.s241099
Cooper, T. G., Noonan, E., Eckardstein, S. von, Auger, J., Baker, H. W. G., Behre, H. M., Haugen, T. B., Kruger, T. F., Wang, C., Mbizvo, M. T., & Vogelsong, K. M. (2009). World Health Organization reference values for human semen characteristics*‡ [Review of World Health Organization reference values for human semen characteristics*‡]. Human Reproduction Update, 16(3), 231. Oxford University Press. https://doi.org/10.1093/humupd/dmp048
Ding, N., Zhang, X., Zhang, X. D., Jing, J., Liu, S. S., Mu, Y., Peng, L. L., Yan, Y. J., Xiao, G. M., Bi, X., Chen, H., Li, F. H., Yao, B., & Zhao, A. Z. (2020). Impairment of spermatogenesis and sperm motility by the high-fat diet-induced dysbiosis of gut microbes. In Gut (Vol. 69, Issue 9, p. 1608). BMJ. https://doi.org/10.1136/gutjnl-2019-319127
Durairajanayagam, D. (2018). Lifestyle causes of male infertility. In Arab Journal of Urology (Vol. 16, Issue 1, p. 10). Elsevier BV. https://doi.org/10.1016/j.aju.2017.12.004
Gabriel, L. K., & Vawda, A. I. (1993). Preparation of Human Sperm for Assisted Conception: A Comparative Study. In Archives of Andrology (Vol. 30, Issue 1, p. 1). Taylor & Francis. https://doi.org/10.3109/01485019308988361
Selvam, M. K. P., Agarwal, A., Pushparaj, P. N., Baskaran, S., & Bendou, H. (2019). Sperm Proteome Analysis and Identification of Fertility-Associated Biomarkers in Unexplained Male Infertility. In Genes (Vol. 10, Issue 7, p. 522). Multidisciplinary Digital Publishing Institute. https://doi.org/10.3390/genes10070522
- Wogatzky, J., Wirleitner, B., Stecher, A., Vanderzwalmen, P., Neyer, A., Spitzer, D., Schuff, M., Schechinger, B., & Zech, N. H. (2012). The combination matters – distinct impact of lifestyle factors on sperm quality: a study on semen analysis of 1683 patients according to MSOME criteria. In Reproductive Biology and Endocrinology (Vol. 10, Issue 1, p. 115). BioMed Central. https://doi.org/10.1186/1477-7827-10-115
Southern California Reproductive Center. (n.d.). CBD and fertility. Southern California Reproductive Center. Retrieved January 30, 2025, from https://www.scrcivf.com/cbd-and-fertility/