

Type 2 Diabetes
AIC’s Type 2 Diabetes bundle is a comprehensive supplement regimen designed to support blood sugar management at its root cause and improve overall health. This bundle combines essential nutrients and antioxidants to boost energy, support digestive health, and promote cardiovascular well-being. With a focus on natural ingredients and holistic wellness, this bundle is perfect for those seeking a balanced approach to diabetes management. Experience the benefits of improved blood sugar control and enhanced overall well-being.
Understanding Type 2 Diabetes Mellitus
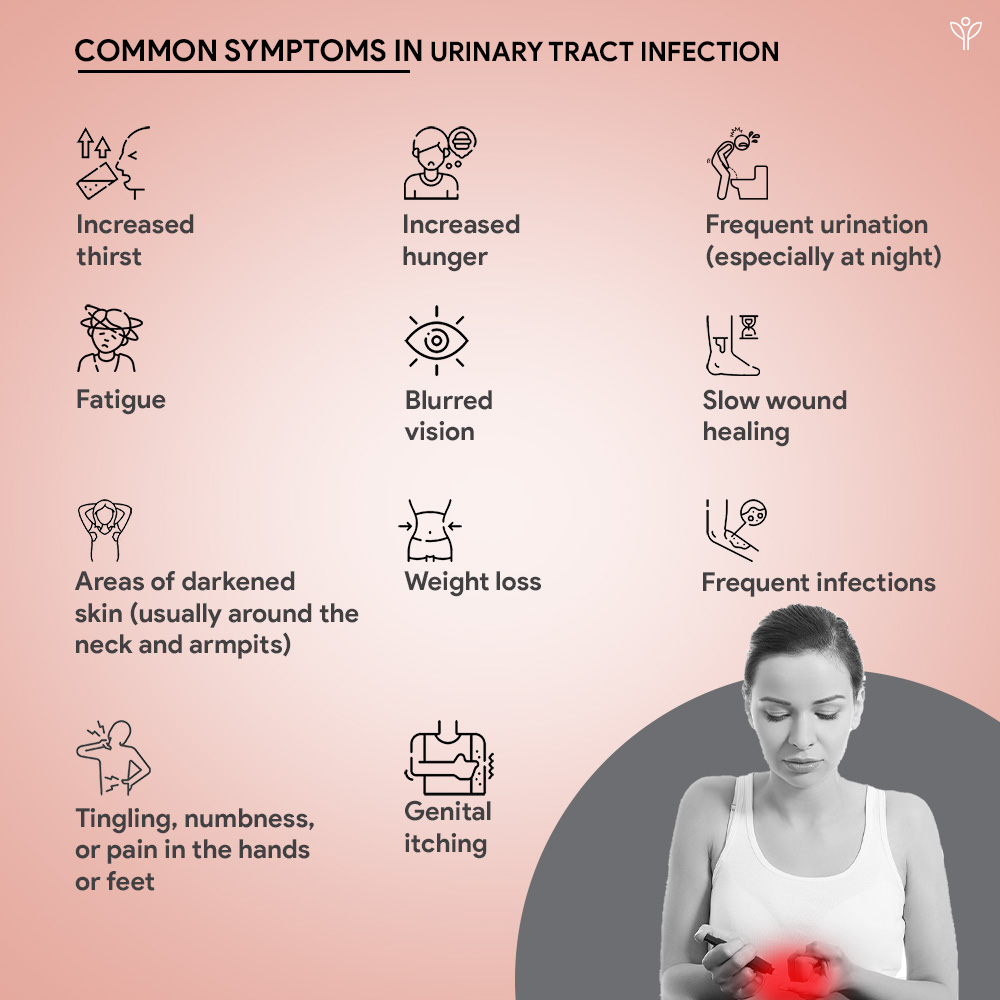
Type 2 Diabetes Mellitus is a chronic disorder characterized by high blood sugar levels. It occurs due to the body’s inability to utilise insulin (a hormone produced by the pancreas to carry sugar into cells for energy) effectively, a condition known as insulin resistance (Kendall et al., 2006) rather than misunderstood as insulin insufficiency. This resistance causes high levels of glucose in blood, which further leads to a number of complications like heart, kidney, vision and nerve problems.
According to the WHO, 830 million people worldwide had diabetes in 2022, a number projected to rise to 1.1 billion by 2045 (Perveen et al., 2019). In 2019, 77 million people were affected by diabetes in India, a figure expected to cross 134 million by 2045. (Mohan & Pradeepa, 2021).

What we have in Type 2 Diabetes
Reference
Chatterjee, S., & Mudher, A. (2018). Alzheimer’s Disease and Type 2 Diabetes: A Critical Assessment of the Shared Pathological Traits [Review of Alzheimer’s Disease and Type 2 Diabetes: A Critical Assessment of the Shared Pathological Traits]. Frontiers in Neuroscience, 12. Frontiers Media. https://doi.org/10.3389/fnins.2018.00383
Deng, Z., Davis, J., Muniz-Rodriguez, F., & Richardson, F. (2018). Successful Management of Poorly Controlled Type 2 Diabetes with Multidisciplinary Neurobehavioral Rehabilitation: A Case Report and Review. In Diabetes Therapy (Vol. 9, Issue 4, p. 1713). Adis, Springer Healthcare. https://doi.org/10.1007/s13300-018-0448-7
Fletcher, B. J., Gulanick, M., & Lamendola, C. (2002). Risk Factors for Type 2 Diabetes Mellitus. In The Journal of Cardiovascular Nursing (Vol. 16, Issue 2, p. 17). Lippincott Williams & Wilkins. https://doi.org/10.1097/00005082-200201000-00003
Karamanou, M. (2016). Milestones in the history of diabetes mellitus: The main contributors [Review of Milestones in the history of diabetes mellitus: The main contributors]. World Journal of Diabetes, 7(1), 1. https://doi.org/10.4239/wjd.v7.i1.1
Jakovljevic, N. K., Pavlović, K., Jotić, A., Lalić, K., Stoiljković, M., Lukić, L., Miličić, T., Maćešić, M., Gajović, J. S., & Lalić, N. (2021). Targeting Mitochondria in Diabetes. In International Journal of Molecular Sciences (Vol. 22, Issue 12, p. 6642). Multidisciplinary Digital Publishing Institute. https://doi.org/10.3390/ijms22126642
Kendall, D. M., Kim, D., & Maggs, D. (2006). Incretin Mimetics and Dipeptidyl Peptidase-IV Inhibitors: A Review of Emerging Therapies for Type 2 Diabetes [Review of Incretin Mimetics and Dipeptidyl Peptidase-IV Inhibitors: A Review of Emerging Therapies for Type 2 Diabetes]. Diabetes Technology & Therapeutics, 8(3), 385. Mary Ann Liebert, Inc. https://doi.org/10.1089/dia.2006.8.385
Krause, M., & Vito, G. D. (2023). Type 1 and Type 2 Diabetes Mellitus: Commonalities, Differences and the Importance of Exercise and Nutrition. Nutrients, 15(19), 4279. https://doi.org/10.3390/nu15194279
Mohan, V., & Pradeepa, R. (2021). Epidemiology of type 2 diabetes in India. In Indian Journal of Ophthalmology (Vol. 69, Issue 11, p. 2932). Medknow. https://doi.org/10.4103/ijo.ijo_1627_21
Olokoba, A. B., Obateru, O. A., & Olokoba, L. B. (2012). Type 2 Diabetes Mellitus: A Review of Current Trends [Review of Type 2 Diabetes Mellitus: A Review of Current Trends]. Oman Medical Journal, 27(4), 269. Oman Medical Specialty Board. https://doi.org/10.5001/omj.2012.68
Ozougwu, O. (2013). The pathogenesis and pathophysiology of type 1 and type 2 diabetes mellitus. Journal of Physiology and Pathophysiology, 4(4), 46. https://doi.org/10.5897/jpap2013.0001
Perveen, S., Shahbaz, M., Keshavjee, K., & Guergachi, A. (2019). Prognostic Modeling and Prevention of Diabetes Using Machine Learning Technique. In Scientific Reports (Vol. 9, Issue 1). Nature Portfolio. https://doi.org/10.1038/s41598-019-49563-6
Pilz, S., Kienreich, K., Rutters, F., Jongh, R. de, Ballegooijen, A. J. van, Grübler, M., Tomaschitz, A., & Dekker, J. (2012). Role of Vitamin D in the Development of Insulin Resistance and Type 2 Diabetes. In Current Diabetes Reports (Vol. 13, Issue 2, p. 261). Springer Science+Business Media. https://doi.org/10.1007/s11892-012-0358-4
Pintaudi, B., Vieste, G. D., & Bonomo, M. (2016). The Effectiveness of Myo-Inositol and D-Chiro Inositol Treatment in Type 2 Diabetes. In International Journal of Endocrinology (Vol. 2016, p. 1). Hindawi Publishing Corporation. https://doi.org/10.1155/2016/9132052
Solomon, T. P. J., Haus, J. M., Kelly, K. R., Cook, M. D., Filion, J., Rocco, M., Kashyap, S., Watanabe, R. M., Barkoukis, H., & Kirwan, J. P. (2010). A low–glycaemic index diet combined with exercise reduces insulin resistance, postprandial hyperinsulinemia, and glucose-dependent insulinotropic polypeptide responses in obese, prediabetic humans. In American Journal of Clinical Nutrition (Vol. 92, Issue 6, p. 1359). Elsevier BV. https://doi.org/10.3945/ajcn.2010.29771