
Urinary Tract Infection
AIC’s Urinary Tract Infection bundle is a comprehensive blend of D-Mannose, Cranberry Extract, Vitamin C, and Probiotics. This powerful formula helps prevent infections and hence UTIs, supports immune function, and promotes a healthy urinary, vaginal and gut microbiome.
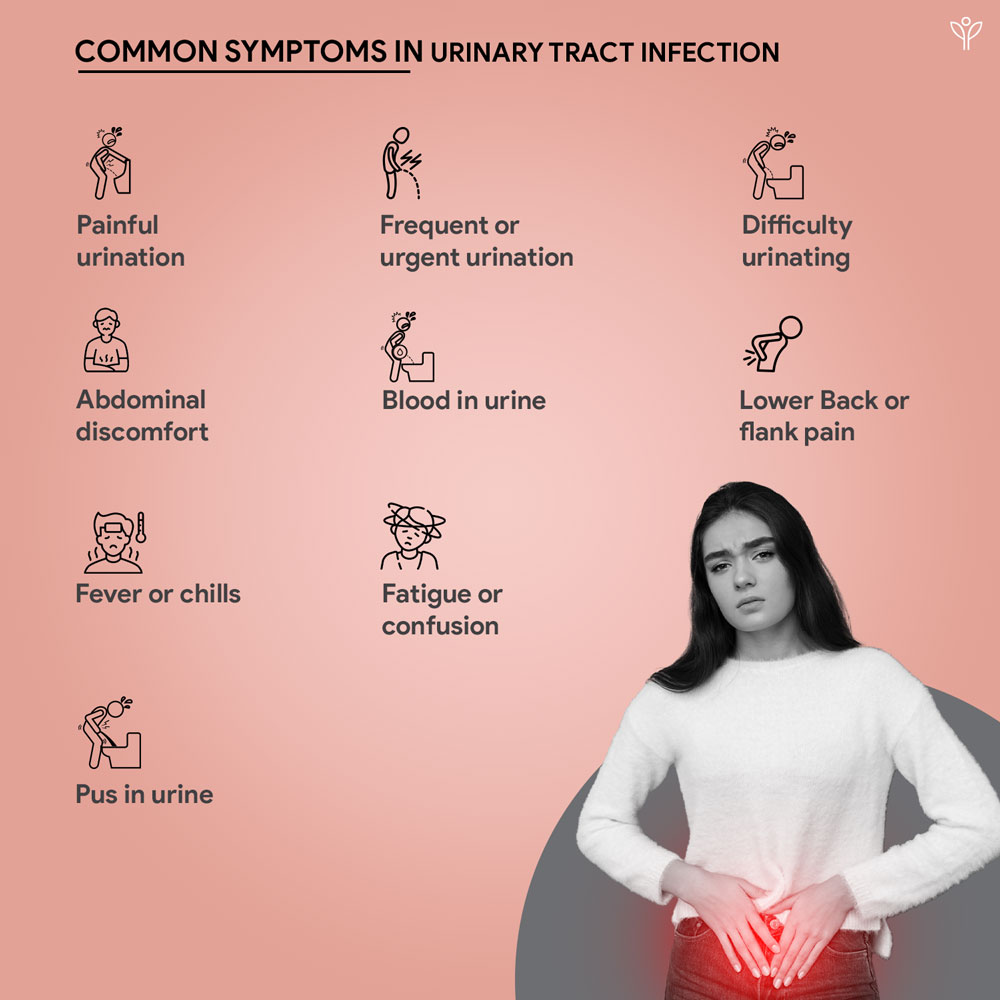
Understanding Urinary Tract Infection (UTI)
A urinary tract infection (UTI) is an infection that affects any part of the urinary tract, which includes the kidneys, ureters, bladder, and urethra.
UTI’s are one of the most common infections that is presented to healthcare providers, with more prevalence amongst women. It is estimated that approximately 40% of women and 12% of men will experience symptoms of a UTI at some point in their lives.

What we have in Urinary Tract Infection
Reference
Foxman, B., Barlow, R., d’Arcy, H., Gillespie, B. W., & Sobel, J. D. (2000). Urinary Tract Infection. In Annals of Epidemiology (Vol. 10, Issue 8, p. 509). Elsevier BV. https://doi.org/10.1016/s1047-2797(00)00072-7
Geerlings, S. E. (2016). Clinical Presentations and Epidemiology of Urinary Tract Infections [Review of Clinical Presentations and Epidemiology of Urinary Tract Infections]. Microbiology Spectrum, 4(5). American Society for Microbiology. https://doi.org/10.1128/microbiolspec.uti-0002-2012
Jauhari, R., Bhatt, M., & Dudeja, P. (2022). An Overview: Antibiotic Sensitive Pattern in Urinary Tract Infection. In International Journal of Pharmaceutical Sciences Review and Research (Vol. 72, Issue 1). https://doi.org/10.47583/ijpsrr.2022.v72i01.016
Cloyd, J. (2023, July 13). A functional medicine UTI protocol: Specialized testing, therapeutic diet, and supplements. Rupa Health. https://www.rupahealth.com/post/a-functional-medicine-uti-protocol-specialized-testing-therapeutic-diet-and-supplements
University of Wisconsin Integrative Health Program. (2021). Integrative approaches for urinary tract infections. University of Wisconsin-Madison.