

Constipation
AIC’s Constipation Wellness bundle is an expertly curated trio of supplements combines the digestive power of Powerful Digestive Enzymes, the biofilm-busting benefits of Biofilm Care, and the immune-boosting properties of Vitamin C Care to help regulate, comfortable bowel movements, ease digestive stress, and promote a healthy gut.
Understanding Constipation
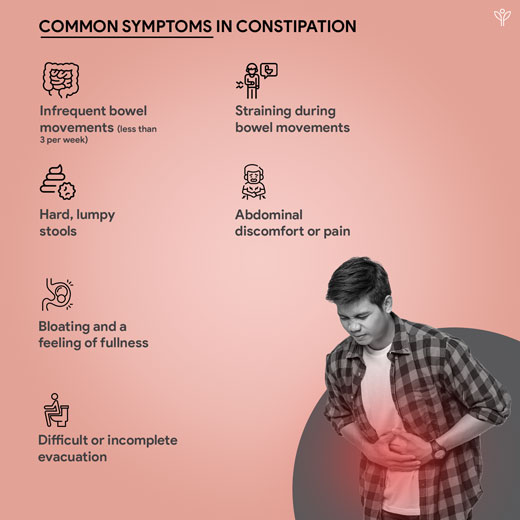
Constipation, a common gastrointestinal condition, is characterized by infrequent or difficult bowel movements, often accompanied by abdominal discomfort.
This complex disorder can be influenced by a variety of factors, including physical, psychological, physiological, emotional, and environmental considerations. (Gattuso & Kamm, 1993) Affecting individuals of all ages, constipation is more prevalent in females, with an estimated prevalence of 15-20% in the general population. (Gattuso & Kamm, 1993) (Rao, 2008).
Defining constipation, the Rome IV criteria categorize disorders of chronic constipation (constipation persisting for more than 3 months) into four subtypes:
- functional constipation
- irritable bowel syndrome with constipation
- opioid-induced constipation
- functional defecation disorders

What we have in Constipation
Reference
Gattuso, J. M., & Kamm, M. A. (1993). The management of constipation in adults [Review of the management of constipation in adults]. Alimentary Pharmacology & Therapeutics, 7(5), 487. Wiley.
Gray, J. R. (2011). What is Chronic Constipation? Definition and Diagnosis. In J. R. Gray, Canadian Journal of Gastroenterology and Hepatology (Vol. 25, p. 7). Pulsus Group.
Hsieh, C. (2005). Treatment of constipation in older adults. In C. Hsieh, PubMed (Vol. 72, Issue 11, p. 2277). National Institutes of Health.
Mari, A., Mahamid, M., Amara, H., Baker, F. A., & Yaccob, A. (2020). Chronic Constipation in the Elderly Patient: Updates in Evaluation and Management. In A. Mari, M. Mahamid, H. Amara, F. A. Baker, & A. Yaccob, Korean Journal of Family Medicine (Vol. 41, Issue 3, p. 139). Korean Academy of Family Medicine.
Rao, S. S. C. (2008). Dyssynergic Defecation and Biofeedback Therapy [Review of Dyssynergic Defecation and Biofeedback Therapy]. Gastroenterology Clinics of North America, 37(3), 569. Elsevier BV.
Rao, S. S. C., & Brenner, D. M. (2021). Efficacy and Safety of Over-the-Counter Therapies for Chronic Constipation: An Updated Systematic Review [Review of Efficacy and Safety of Over-the-Counter Therapies for Chronic Constipation: An Updated Systematic Review]. The American Journal of Gastroenterology, 116(6), 1156. Lippincott Williams & Wilkins.
Somes, J., & Donatelli, N. S. (2013). Constipation and the Geriatric Patient: Treatment in the Emergency Department [Review of Constipation and the Geriatric Patient: Treatment in the Emergency Department]. Journal of Emergency Nursing, 39(4), 372. Elsevier BV.