

Fatty Liver
AIC’s Fatty Liver Wellness bundle supports your liver and it’s natural detoxification to help address fatty liver and its root causes. This expertly curated combination of supplements is designed to reduce inflammation, improve insulin sensitivity, support liver detoxification, and promote optimal liver function.
Understanding Fatty Liver
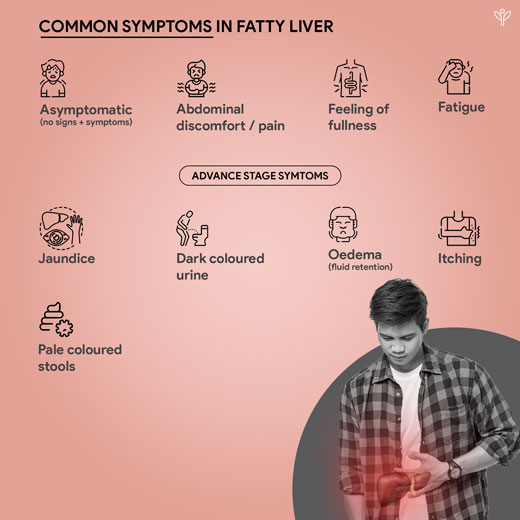
Fatty liver can be defined as the accumulation of excess fat in the liver, specifically triglycerides, which can lead to a range of liver diseases if left untreated (Korish & Arafah, 2013). It may be divided into two main types: alcoholic fatty liver disease and non-alcoholic fatty liver disease.
Alcoholic fatty liver disease –
In this condition, excess alcohol consumption leads to the buildup of fat in the liver. This replacement of liver cells by fat can lead to steatohepatitis, cirrhosis, and even liver failure.
Non-alcoholic fatty liver disease (NAFLD) –
On the other hand, non-alcoholic fatty liver disease is characterized by the accumulation of fat in the liver in the absence of significant alcohol consumption. This condition is closely linked to metabolic syndrome (high blood pressure, high blood sugar and weight gain), obesity, insulin resistance, and dyslipidaemia. (Korish & Arafah, 2013) (Ju et al., 2020) (Gusdon et al., 2014) NAFLD includes both simple fatty liver (NAFL) and non-alcoholic steatohepatitis (NASH).

What we have in Fatty Liver
Reference
Ciardullo, S., Muraca, E., Vergani, M., Invernizzi, P., & Perseghin, G. (2023). Advancements in pharmacological treatment of NAFLD/MASLD: a focus on metabolic and liver-targeted interventions. In Gastroenterology report (Vol. 12).
Conlon, B. A., Beasley, J. M., Aebersold, K., Jhangiani, S. S., & Wylie‐Rosett, J. (2013). Nutritional Management of Insulin Resistance in Nonalcoholic Fatty Liver Disease (NAFLD) [Review of Nutritional Management of Insulin Resistance in Nonalcoholic Fatty Liver Disease (NAFLD)]. Nutrients, 5(10), 4093. Multidisciplinary Digital Publishing Institute.
Diehl, A. M., Clarke, J., & Brancati, F. L. (2003). Insulin Resistance Syndrome and Nonalcoholic Fatty Liver Disease. In Endocrine Practice (Vol. 9, p. 93). Elsevier BV.
Gusdon, A. M., Song, K., & Qu, S. (2014). Nonalcoholic Fatty Liver Disease: Pathogenesis and Therapeutics from a Mitochondria-Centric Perspective [Review of Nonalcoholic Fatty Liver Disease: Pathogenesis and Therapeutics from a Mitochondria-Centric Perspective]. Oxidative Medicine and Cellular Longevity, 2014, 1. Hindawi Publishing Corporation.
Hendriks, D., Brouwers, J. F., Hamer, K. M., Geurts, M. H., Luciana, L., Massalini, S., López‐Iglesias, C., Peters, P. J., Colman, M. J. R., Lopes, S. M. C. de S., Artegiani, B., & Clevers, H. (2023). Engineered human hepatocyte organoids enable CRISPR-based target discovery and drug screening for steatosis. In Nature Biotechnology (Vol. 41, Issue 11, p. 1567). Nature Portfolio.
Ju, U.-I., Jeong, D.-W., Seo, J., Park, J. B., Park, J., Suh, K., Kim, J. B., & Chun, Y. (2020). Neddylation of sterol regulatory element-binding protein 1c is a potential therapeutic target for nonalcoholic fatty liver treatment. In Cell Death and Disease (Vol. 11, Issue 4). Springer Nature.
Korish, A. A., & Arafah, M. (2013). Camel milk ameliorates steatohepatitis, insulin resistance and lipid peroxidation in experimental non-alcoholic fatty liver disease. In BMC Complementary and Alternative Medicine (Vol. 13, Issue 1). BioMed Central.